- प्रोडक्ट्स
- हेल्थ और वेलनेस प्लान
- Comprehensive Product + PortUp to 100% premium back + Durable equipment cover + Up to 5-year tenure₹9,952*/वर्षविवरण देखें
- Comprehensive ProductHealthReturns™ + No Capping on Medical Expenses + Super Reload₹6,177*/वर्षविवरण देखें
- Tailored ProductHealthReturns™ + No Capping on Medical Expenses + Super Reload₹5,630*/वर्षविवरण देखें
- Max Protection + ChronicHealthReturns™ + Day 1 Cover for 7 Conditions + Chronic Management Program ₹7,111*/वर्षविवरण देखें
- अधिकतम सुरक्षाUp to Rs. 95* lakh coverage with an affordable premium₹962*/वर्षविवरण देखें
- अधिकतम सुरक्षाHealth Insurance + Health Benefits + Rewards₹6,863*/वर्षविवरण देखें
*वेबसाइट पर दिए गए प्लान की शुरुआती कीमत 30 वर्ष की आयु के कस्टमर और 5 लाख के सम इंश्योर्ड के लिए है.
#5% discount from 4th policy year to 7th policy year. 10% discount from 8th policy onwards, will be available at renewal.
- Large payout plans
- एक्सीडेंट के लिए हेल्थ इंश्योरेंस कवर₹212*/वर्षविवरण देखें
- कैंसर के खिलाफ कवर के लिए हेल्थ इंश्योरेंस₹428*/वर्षविवरण देखें
- गंभीर बीमारी के बाद आपके भविष्य की सुरक्षा₹5,463*/वर्षविवरण देखें
*वेबसाइट पर दिए गए प्लान की शुरुआती कीमत 30 वर्ष की आयु के कस्टमर और 5 लाख के सम इंश्योर्ड के लिए है.
#5% discount from 4th policy year to 7th policy year. 10% discount from 8th policy onwards, will be available at renewal.
- कॉर्पोरेट प्लान
- Comprehensive corporate health insurance planविवरण देखें
- Fixed benefit plans including personal accident insurance, critical illness insurance and hospital cash benefitविवरण देखें
- The perfect travel insurance planविवरण देखें
*वेबसाइट पर दिए गए प्लान की शुरुआती कीमत 30 वर्ष की आयु के कस्टमर और 5 लाख के सम इंश्योर्ड के लिए है.
#5% discount from 4th policy year to 7th policy year. 10% discount from 8th policy onwards, will be available at renewal.
- इंटरनेशनल कवर
- Avail cashless treatment internationally with this plan₹12,917*/वर्षविवरण देखें
*वेबसाइट पर दिए गए प्लान की शुरुआती कीमत 30 वर्ष की आयु के कस्टमर और 5 लाख के सम इंश्योर्ड के लिए है.
#5% discount from 4th policy year to 7th policy year. 10% discount from 8th policy onwards, will be available at renewal.
- सभी देखेंअभी अप्लाई करें
- वापस जाएं
- हेल्थ और वेलनेस प्लान
- Health Corner
- क्लेम
- हॉस्पिटल नेटवर्क
- तुरंत कोटेशन प्राप्त करें
- ग्राहक सहायता
- मेरा अकाउंट
मेरी प्रोफाइल
ज़रूरी लिंक्स
Grievance
- सहायता
- Create your Health ID
- कॉर्पोरेट
- Become an Advisor
- व्हॉट्सऐप
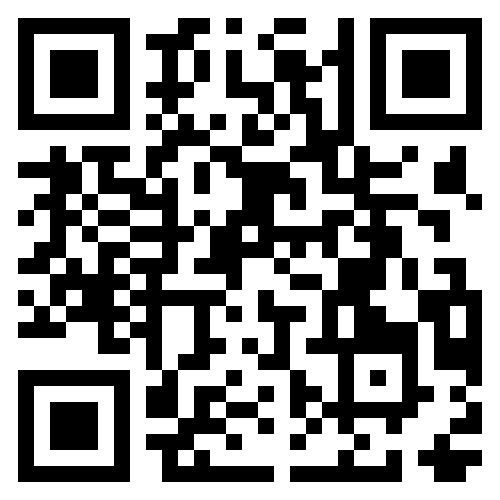
- Port in to ABHI
- हमसे संपर्क करें
- Self Servicing
- वापस जाएं
- मेरा अकाउंट





 1800-270-7000
1800-270-7000