For people with or at risk of diabetes, understanding skin diabetes symptoms is a vital part of everyday self-care. It helps you:
- Spot changes early
- Seek timely medical advice
- Protect your long-term health, including serious complications
A robust health insurance plan, such as those from Aditya Birla Health Insurance, can ensure easier access to dermatologists, blood tests, and long-term management when skin problems due to diabetes arise.
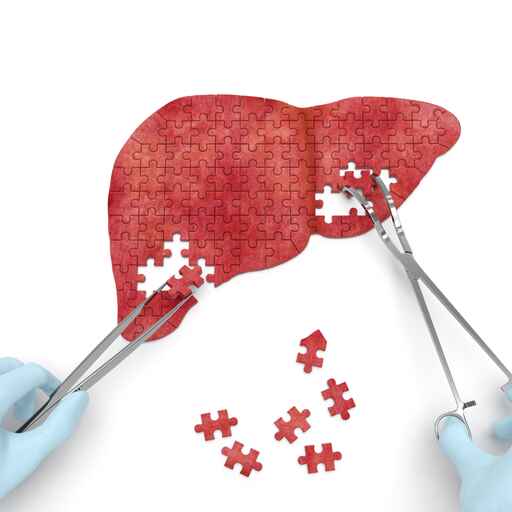
How Diabetes Affects Your Skin
Diabetes affects how your body uses insulin and controls blood sugar. When blood sugar stays high over time, it can:
- Damage small blood vessels and nerves that supply your skin
- Reduce blood flow, especially to your legs and feet
- Lower your body’s ability to fight infections
- Causes dehydration, which leads to dry, itchy skin
Early Skin Diabetes Symptoms You Should Watch For
Some skin changes are subtle and easy to ignore. However, they can be early signs of diabetes or prediabetes and should never be overlooked.
Watch out for:
- Unusual dryness and itchiness
- Dark, velvety patches
- Shiny, reddish-brown patches on the shins
- Frequent skin infections
- Slow-healing cuts, cracks, or sores
- Thick, tight, or waxy skin on the hands, fingers, or toes
If you notice any of these early skin diabetes symptoms, it is important to speak to your doctor and get your blood sugar checked.
Common Diabetic Skin Conditions (With Causes & Treatment)
Below are some of the most recognised diabetic skin conditions, how they develop, and what you can do about them.
Acanthosis Nigricans (Dark, Velvety Skin Patches)
Acanthosis nigricans causes dark, thick, velvety patches on body folds such as the neck, armpits, or groin. It is often one of the earliest visible signs of insulin resistance.
What Causes It
- Strongly linked to insulin resistance, prediabetes, and type 2 diabetes
- More common in people who are overweight or obese
What to Do
- Get screened for diabetes and other metabolic conditions
- Work with your doctor on weight management, diet, and exercise
- Use prescribed creams only if recommended, as cosmetic lightening alone does not treat the cause
Diabetic Dermopathy (Shin Spots)
Diabetic dermopathy appears as light brown, round or oval, slightly scaly patches on the shins. They are sometimes called “shin spots.”
What Causes It
- Long-standing diabetes affects small blood vessels in the skin
- Minor trauma to the shins combined with poor circulation
What To Do
- Usually does not need specific treatment and may fade over time
- Focus on good blood sugar control
- Protect your legs from bumps and injuries
Necrobiosis Lipoidica
Necrobiosis lipoidica causes yellow-brown, shiny patches, often on the front of the shins.
What Causes It
- Changes in collagen and blood vessels in people with diabetes
- More common in adult women and in those with long-standing disease
What to Do
- See a dermatologist early to prevent ulcers
- Avoid scratching or injuring affected areas
- Your doctor may recommend topical or injected medicines to reduce inflammation
Bullosis Diabeticorum (Diabetic Blisters)
These are spontaneous, painless blisters that appear on the hands, feet, legs, or forearms.
What Causes It
- Seen in people with long-standing diabetes, especially with neuropathy
- The exact cause is unclear, but linked to fragile skin and poor microcirculation
What to Do
- Do not burst the blisters yourself
- Keep them clean, dry, and protected to prevent infection
- Seek medical advice, especially if there is redness, pain, or discharge
Eruptive Xanthomatosis
This condition causes small, yellowish, pimple-like bumps with a red base, often on the buttocks, thighs, or elbows.
What Causes It
- Very high triglyceride levels
- Poorly controlled diabetes or underlying lipid disorders
What to Do
- Immediate medical review to check sugar and cholesterol levels
- Medication and lifestyle changes to control lipids and blood sugar
- Lesions often clear once levels are brought under control
Digital Sclerosis (Thick, Waxy Skin)
Digital sclerosis makes the skin on the fingers, hands, and sometimes toes feel thick, tight, and waxy. Joint stiffness can also occur.
What Causes It
- Long-term high blood sugar affects collagen in the skin
- Often associated with other diabetes complications
What to Do
- Optimise blood sugar control
- Use emollients to soften the skin
- Physiotherapy or hand exercises may help maintain flexibility
Bacterial Infections
People with diabetes are more prone to bacterial infections such as boils, styes, folliculitis, or infected cuts. The skin may be red, hot, swollen, and painful.
What Causes It
- High blood sugar provides a favourable environment for bacteria
- Reduced immune response and poor circulation
What to Do
- Do not delay seeing a doctor if you notice pain, warmth, pus, or fever
- You may need antibiotic creams or tablets
- Keep blood sugar under control to reduce the risk of recurrence
Fungal Infections
Fungal infections, especially from Candida, can cause red, itchy rashes in warm, moist areas like under the breasts, in the groin, or between fingers and toes.
What Causes It
- High blood sugar and sweat create ideal conditions for fungi
- Common in skin folds and under tight clothing
What to Do
- Use doctor-recommended antifungal creams or powders
- Keep skin folds clean, dry, and well-ventilated
- Review your diabetes control and lifestyle factors
Dry and Itchy Skin
Dry, itchy skin is one of the most frequent skin problems due to diabetes, especially on the legs, arms, and feet.
What Causes It
- Dehydration and poor blood flow to the skin
- Frequent urination, high blood sugar, and damage to nerves
What to Do
- Use gentle, fragrance-free moisturisers daily
- Avoid very hot showers and harsh soaps
Discuss persistent itching with your doctor, as it may signal other complications
Frequently Asked Questions
Early signs may include unusual dryness and itching, dark velvety patches on the neck or armpits, small shiny patches on the shins, or frequent skin infections.
Yes. Diabetes can cause dry, itchy skin, fungal rashes in skin folds, and inflammatory conditions like necrobiosis lipoidica or diabetic dermopathy that appear as discoloured patches.
You cannot be sure on your own. If you have risk factors, a prior diabetes diagnosis, or multiple unexplained skin changes, consult your doctor for blood sugar tests and a proper skin examination.
Some conditions improve with better blood sugar control, while others may leave colour or texture changes. Early treatment and regular follow-up can reduce long-term marks and complications.
Yes. Persistently high blood sugar weakens immunity, slows healing, and increases the risk of infections and chronic skin changes, especially on the legs and feet.
In many cases, yes. Good glycaemic control, healthy lifestyle changes, and appropriate skin treatment can significantly improve or even clear several diabetes-related skin conditions over time.





 1800-270-7000
1800-270-7000